In the high-stakes world of healthcare documentation, the difference between a patient's recovery and a tragic medical error often rests on the placement of a single decimal point or the interpretation of a lone letter. For decades, medical shorthand was the grease that kept the wheels of clinical workflow turning, allowing doctors to dictate or scribble orders at lightning speed. However, as patient safety became a global priority, the risks associated with these shortcuts became impossible to ignore. The Joint Commission (JC), the primary accrediting body for healthcare organizations in the United States, established an Official "Do Not Use" List to eliminate the most dangerous abbreviations. For transcriptionists and healthcare documentation specialists, adhering to these guidelines is not just a matter of stylistic preference; it is a fundamental safety protocol designed to save lives.
The "Do Not Use" List: Targeting the Most Dangerous Offenders
The Joint Commission’s "Do Not Use" list targets abbreviations that have a high statistical correlation with medication errors. At the top of this list is the abbreviation "U" or "u" for units. While it seems harmless, it is frequently misread as the number "0" (zero), "4" (four), or even "cc" (cubic centimeters). An order for "10U" of insulin can easily be misinterpreted as "100" units—a tenfold overdose that can be fatal. Consequently, transcription guidelines mandate that "unit" must always be written out in full. Similarly, "IU" (International Unit) is often mistaken for "IV" (intravenous) or the number "10," leading to incorrect administration routes or dosages.
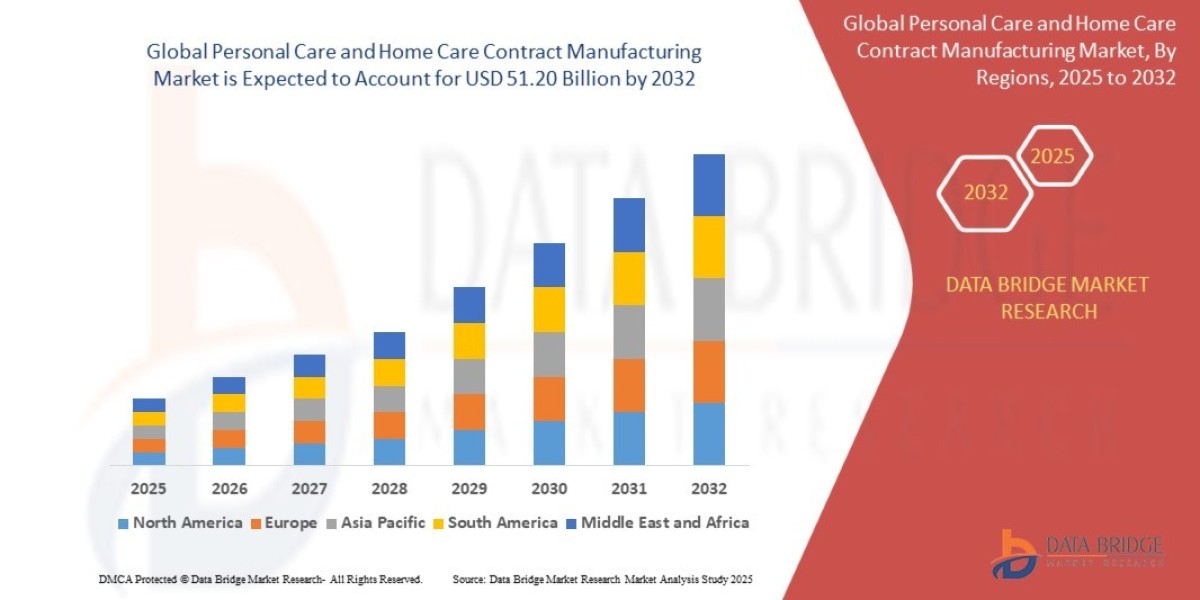
The Danger of Decimals: Trailing and Leading Zeros
Numerical notation is another high-risk area where The Joint Commission has set strict boundaries. The two major culprits are the "trailing zero" and the "lack of a leading zero." A trailing zero occurs when a whole number is followed by a decimal and a zero, such as "5.0 mg." If the decimal point is missed or obscured, the dose is read as "50 mg." Conversely, a leading zero refers to a decimal dose less than one, such as ".5 mg." If the decimal is missed here, the dose is read as "5 mg." The JC requirement is clear: never use a trailing zero for whole numbers, and always use a leading zero for decimal values.
[Image showing the correct vs. incorrect use of decimal points in medication dosages: 5 mg instead of 5.0 mg, and 0.5 mg instead of .5 mg]
In the context of a professional audio typing course, transcriptionists are trained to automatically correct these numerical risks. Even if a physician dictates "five point zero milligrams," the typist should transcribe it as "5 mg" to prevent the decimal from being overlooked in a printed or digital chart. This "silent correction" is part of the expertise that documentation specialists bring to the table. By adhering to the rule of "X mg" and "0.X mg," they ensure that the dosage is unmistakable. This meticulous attention to detail is what separates a standard typist from a specialized medical documentation professional who understands the clinical implications of their work.
Confusion Between Chemical Symbols and Drug Names
Beyond units and dosages, certain drug names and chemical symbols are notorious for causing confusion. The Joint Commission and the Institute for Safe Medication Practices (ISMP) strongly discourage the use of "MS," "MSO4," and "MgSO4." These abbreviations are frequently confused with one another; "MS" and "MSO4" can mean morphine sulfate, while "MgSO4" stands for magnesium sulfate. Confusing a potent opioid like morphine with a mineral like magnesium sulfate can result in profound patient harm, including respiratory depression or cardiac issues. The safe practice is to always write out the full drug name: "morphine sulfate" or "magnesium sulfate."
Transcriptionists must be hyper-vigilant when listening to audio that contains these sounds. A well-rounded audio typing course provides the phonetic training necessary to distinguish between similar-sounding drug names and the context clues needed to identify the intended medication. For example, if a physician is discussing pain management, "MS" likely refers to morphine, but the transcriptionist must still expand the term to be compliant. This proactive approach to documentation ensures that the final report is a high-fidelity representation of the physician's clinical intent, presented in a format that meets the highest regulatory standards of the modern healthcare facility.
Standardizing Symbols and Apothecary Units
The use of symbols like ">" (greater than), "<" (less than), and "@" (at) also falls under the "Do Not Use" umbrella for certain institutions, as they can be mistaken for numbers or letters. The symbol ">" might be misread as a "7," and "@" can look like a "2." Similarly, "cc" is a legacy term that should be replaced with "mL" or "milliliters," as "cc" can be mistaken for "U" (units) when written or read quickly. Apothecary units, such as "dr" (dram) or "min" (minim), are also being phased out in favor of metric units to prevent confusion among practitioners who are primarily trained in the metric system.
For those looking to enter the field, an audio typing course serves as the training ground for these standardized conversions. Typists learn to listen for "cc" and instinctively type "mL." They learn to replace the "@" symbol with the word "at." This standardization is vital as medical records are increasingly shared across different departments and healthcare systems. When every document follows the same set of rules, the likelihood of a communication breakdown decreases significantly. The goal is to create a universal language of documentation that is as transparent and error-proof as possible, ensuring that every member of the care team is on the same page.
Conclusion: The Transcriptionist as a Guardian of Safety
The evolution of medical documentation has shifted the role of the transcriptionist from a passive observer to an active participant in patient safety. By strictly following the Joint Commission guidelines for the expansion of high-risk abbreviations, documentation specialists prevent the "Swiss Cheese Model" of accidents, where small errors align to create a major failure. The "Do Not Use" list is not a suggestion; it is a vital tool in the arsenal of a professional audio typist.